
Asymptomatic bacteriuria in postmenopausal women with diabetes mellitus
Article authors




1Urology Department of Moscow State University of Medicine and Dentistry, Moscow, Russian Federation
2Endocrinology Department of First Moscow State University of Medicine, Moscow, Russian Federation
3Pirogov Russian National Research Medical University, Department of Endocrinology and Diabetology, Moscow, Russian Federation
Introduction. An evaluation of efficacy of the management of urinary tract infections by using local forms of Estriol in postmenopausal women with type II diabetes and asymptomatic bacteriuria.
Material and methods. The study was conducted in two stages. The first stage: a prospective cross– sectional study to identify patients with asymptomatic bacteriuria. During this stage, 414 postmenopausal women with type II diabetes, but without clinical symptoms of urinary tract infection, were investigated. In the second stage, women with asymptomatic bacteriuria (87 women) were randomized to two groups: the first group was the main group receiving 0.5 mg of Estriol as a vaginal cream, the second group was the control group. The study lasted 12 months.
Results. After 12 months of the study, asymptomatic bacteriuria was revealed in 19.4% of women in the group 1 and 68.4% of women in the group 2 (р < 0.001), and symptomatic urinary tract infection in 8.3% of women in the group 1 and 18.4% of women in the group 2 (р < 0.001). There was no connection revealed between asymptomatic bacteriuria and НвА1с. Using Estriol in group 1 led to an increase in VHI, the appearance of lactobacilli in the vaginal smear, and the decrease of symptom frequency in atrophic vaginitis. In group 2, there were no significant changes revealed.
Conclusions. Usage of local forms of Estriol effectively prevents and decreases the frequency of asymptomatic bacteriuria and urinary tract infection in postmenopausal women suffering with diabetes mellitus.
Key Words: asymptomatic bacteriuria, urinary tract infections, diabetes mellitus, postmenopause
INTRODUCTION
The necessity to treat asymptomatic bacteriuria (AB) in women with type II diabetes is a problem, which could be called unsolved since the analyses of current data on usage of traditional treatment strategy. Particularly antibacterial therapy shows limited efficacy in such patients [1].
The importance of that problem is determined, first of all, both by high prevalence of AB among women [2, 3], as well as by high prevalence of type II diabetes among postmenopausal women [4]. According to some authors, the necessity to treat AB in patients with type II diabetes is related to the risk of the development of upper and lower urinary tract infections (UTI) [4, 5], consequently, taking into consideration the seriousness of potential risks, the principles of treatment are the same as in case of symptomatic urinary tract infections – antibacterial therapy. However, in spite of the current data on development of complications in AB, the need to treat AB for prevention of UTI continues to be actively discussed.
There is a current opinion in the literature that prescription of antibiotics in AB makes sense only in the case of additional factors of UTI development, such as a need for catheterization and urinary tract structural anomalies. In other cases, as it was shown in the large number of studies, an antimicrobial treatment in AB does not lead to decreasing of the frequency of recurrences and re–infections.
Thus, the study conducted by Harding G. [6], where the effectiveness of antimicrobial therapy in women with AB and type II diabetes were investigated, showed that after 4 weeks of a 6–week antimicrobial regimen, AB continued in 20% of patients with diabetes in the group receiving antimicrobial therapy and in 78% of patients in placebo group.
At 27–month follow–up, there was minimum one episode of urinary tract infection in 40% of women in placebo group and in 42% of women receiving antibiotics [7]. The retrospective analysis of studies conducted during period from 1967 to April 2003 showed no evidence of effectiveness of antibiotic use in AB [8]. A fundamentally different approach to prevent recurrent UTI in postmenopausal women is an estrogen regimen. Age–related changes in tissues of the urogenital tract, connected with the development of deficiency of sex hormones after menopause, play a leading role in development of urogenital problems. Inefficiency of antimicrobial therapy in postmenopausal women with diabetes probably relates to the underestimated progressive atrophy of the vaginal mucosa and urinary tract. Studies of the risk factors of AB development in women with diabetes show a significant correlation between age and frequency of bacteriuria.
There were no studies on the use of local forms of hormonal therapy in women with type II diabetes for treatment of AB and prevention of lower urinary tract symptoms (LUTS).
Aim of the current study was an assessment of the possibility of prevention of urinary tract infections by using the local forms of Estriolin in postmenopausal women with diabetes and AB.
MATERIALS AND METHODS
According to the aims, there are two stages emphasized in the study. The first stage – a prospective cross–sectional study revealing AB cases. The second stage – randomized case–control prospective cohort study for assessment of the effectiveness and eligibility of the use of local forms of Estriol for treatment of AB and for prevention of symptomatic forms of UTI. Postmenopausal women with type II diabetes, normoglycemic, without symptomatic signs of UTI participated in the study. The quantitative count of ≥105 cfu/ml of an organism in a voided urine specimen without urinary tract symptoms was accepted as AB [9].
Inclusion criteria were limited to:
- Diabetes type II
- Normoglycemia
- Postmenopausal period
Exclusion criteria were limited to:
- Diabetes type 1
- Significant decompensation of diabetes (HBA1C ≥10%) ) and lack of self–control skills – Glycosuria at time of the study – Symptomatic UTI – Autonomic diabetic polyneuropathy
- Estrogen dependent tumors
- Taking replacement hormonal therapy by sex steroids
- Anatomical defects of the genitourinary system
- Chronic kidney and liver failure
The study was performed after obtaining the consent from the patients and approval of the local Ethics Committee.
At the first stage, after assessing the compliance to inclusion–exclusion criteria, all patients undergone common clinical and microbiological analyses of the urine to reveal AB.
Bacteriological investigation of urine was carried out by standard method accepted in the clinic: midstream urine, taken after hygienic processing of the vulva, was planted by dimensional loop (0.01 ml) on Petri dishes with blood agar and Levin’s medium (Bekton– Dikinson, USA). After incubation at 35°C over 18 hours, the quantity of microbes per 1ml of urine was recalculated based on the number of grown colonies and volume of seeded fluid. Identification and sensitivity of the microbes to antibiotics were carried out on automated microbiological system FENIX 100 (Bekton Dikinson, USA)
In some bacilli, the testing on sensitivity was carried out using a disk–diffusion method in accordance with current standards.
The diagnoses of AB confirmed detecting the same strain of bacilli in the amount of 105 (100,000) and more CFU/ml (colony–forming units) in two consecutive urine analyses.
After confirming the diagnoses of AB, screened women were consistently randomized to two groups by block randomization technique. The treatment method was chosen according to admission date and was changed on a weekly basis.
Women taking local estriol as a vaginal cream containing 0.5 mg of estriol daily at night during three weeks with subsequent transition to the maintenance therapy – twice a week during 12 months – were included into the first (main) group.
Women with natural follow of AB without taking any preventive therapy were included into the second (control) group.
At the second stage of the study, screened women underwent gynecological investigation; colposcopy; calculation of the index of vaginal health: elasticity, transudate, pH, epithelial integrity, humidity [7]; mirror examination of the cervix; and Pappanikolau’s smear from the upper third of the vaginal wall. Studying of the vaginal culture included complex investigation of the vaginal smear, which was based on culture and microscopy of the vaginal smear colored by Gram stain. Vaginal secretion on the swab, brought to the laboratory in a tube with transport medium, was plated to the special mediums: blood agar, Levin’ media, mannitol–salt agar (Staphylococci), bilious–esculin agar (Enterococci), Sabouraud’s agar with chloramphenicol and gentamicin (Fungi). All mediums are manufactured by Bekton– Dikinson, USA.
At the beginning and after 3, 6, and 12 months of therapy, urine common and microbiological analyses, as well as bacteriological analysis of vaginal microflora were conducted, the degree of atrophy of vaginal mucosa was assessed, the vaginal health index as well as the vaginal pH were measured. Patients’complaints and the degree compensation of type II diabetes by the level of HbA1c were assessed. Upon identifying the symptomatic urinary tract infections, the antimicrobial therapy (pefloxacin, 800 mg/day during 7 days) was prescribed to the patients during the study; in case of nonspecific vaginitis, Nifuratel suppositories were used; in case of bacterial vaginosis, clindamycin cream, and vaginal candidiasis was managed by fluconazole. After completion of the therapy the patients continued to be studied.
Statistical analysis
Statistical analysis of the results was done using statistical package Epi Info Software 3.4.3.
Indicators, expressed by quantified continuous variables, were presented as means ± standard deviation (M ±SD). Analysis of distribution of indicators’ values for compliance with the law of normal distribution was carried out using a test Shapiro–Wilk.
Statistical significance assessment of intra– and inter–group differences of quantitative indicators was carried out using Student’s t–criterion, Mann– Whitney U–criterion and criterion of Wilcoxon Mc– Nemar.
A comparison of quality indicators in independent collections was produced by χ2 criterion and Fisher’s exact criterion. To describe the relationship between variables, Spearman rank correlation coefficient (rs) was calculated. Level of statistical significance was accepted at p ≤0.05.
RESULTS
At the first stage of the study during the screening on AB, 414 women without symptomatic UTI were examined. At once collected microbiological analysis of urine, bacteriuria in the amount of 105 or more CFU / ml was detected in 135 (32.6%) of women.
With repetition of the microbiological analysis of urine in patients with once detected bacteriuria after 7–10 days, 41 (9.9%) women had received a normal urinalysis. Between the first and second urine analysis the patients did not receive antibiotics, but were re–instructed on technique of urine collection. After two series of urine analysis, with an interval of 7–10 days, AB was diagnosed in 94 (22.7%) of the 414 patients.
In the second phase of the study, seven of 94 patients were unable to continue the study because of discrepancy of inclusion–exclusion criteria. The 87 women who were able to continue the study were randomly assigned to two groups.
Later, during the study, 9 patients were excluded from the group I and five patients were excluded from group II. The reason for premature exception was violation of the study protocol. Thirty–four patients in the main group and 39 patients in the control group managed fully to complete the study, going through all its stages. Follow–up visits were carried out at 3, 6, and 12 months from the start of the study. However, in this article, the initial and final results are mainly represented. Both groups of patients were matched by age, duration of diabetes and menopause, as well as by the incidence of arterial hypertension, diabetic retinopathy, nephropathy, and peripheral neuropathy. Clinical characteristics of patients are presented in Table 1. The initial level of glycated hemoglobin did not differ in both groups and was 8.61 ±2.03 in the main group and 8.58 ±1.99 in the control group. However, at the beginning of the study, all women had achieved normoglycemia: fasting glucose was until 6 mmol/l, postprandial – until 8 mmol/l. Characteristics of the initial glucose–lowering therapy is shown in table 2, with no statistically significant differences revealed in the methods of glucose–lowering therapy at the time of inclusion into the study. Later, during the study, the principle of glucose–lowering therapy did not fundamentally change; the doses of hypoglycemic agents based on self–control results presented by patients at their visits were corrected.
Table 1. Characteristics of patients included in the study
| Indicator | Group I (n = 43), n (% or М ±SD) | Group II (n = 44), n (% or М ±SD) | p |
| Age (years) М ±SD | 59.7 ±5.7 | 60.2 ±5.3 | 0.683 |
| Duration of diabetes (years) М ±SD | 8.7 ±6.8 | 8.8 ±6.0 | 0.997 |
| Duration of menopause (years) М ±SD | 10.1 ±5.3 | 10.7 ±5.3 | 0.591 |
| Level of HbA1c. М ±SD | 8.61 ±2.03 | 8.58 ±1.99 | 0.942 |
| Arterial hypertension | 86.0% | 88.6 | 0.967 |
| Diabetic retinopathy | 37.2 | 36.4 | 1.000 |
| Diabetic nephropathy | 46.5 | 47.7 | 1.000 |
| Diabetic polyneuropathy | 76.7 | 77.3 | 1.000 |
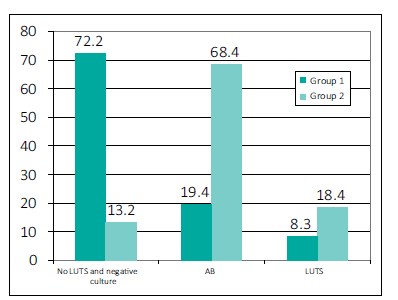
Figure 1. The incidence of AB and UTI after 12 months from the start of the study.
Table 2. Initial characteristics of glucose–lowering therapy and the state of carbohydrate metabolism
| Indicator/Treatment | Main group (n = 43) |
Control group (n = 44) |
р |
| HbA1c. % | 8.61 ±2.03 | 8.58 ±1.99 | 0.942 |
| Sulfonylurea | 5 | 6 | 0.854 |
| Sulfonylurea + metformin | 9 | 12 | 0.854 |
| Combined therapy | 18 | 15 | 0.854 |
| Insulin | 11 | 11 | 1.000 |
At the beginning of the study, all patients were diagnosed with AB, but clinical forms of UTI were excluded After 12 months of the beginning of the treatment, a decrease of the frequency of AB to 19.4% and symptomatic UTI to 8.3% was detected in patients of the main group. In the control group, AB was detected in 68.4% of patients, and symptomatic UTI in 18.4% (p < 0.001) (Figure 1). However, during the study we did not reveal any relations between level of HBA1C and frequency of AB. At the end of the study HBA1C was ≥7.5% in 13 (36.1%) of patients in main group, AB was revealed in 7 (19.4%) of patients, AB was diagnosed in 26 (68.4%) (p < 0.001) of patients in control group in spite of the fact that HBA1C at the 9th months was ≥7.5% in 12 (31.6%) of patients (Table 3).
There were no differences in bacterial composition of urine in women of both groups. E.coli was revealed in 62.5% of patients in the main group, staphylococci in 10%, streptococci in 12.5%, and microbial associations in 15% of patients. In the control group, mentioned microorganisms were detected in 64.1%, 12.1%, 11.8%, and 12% of patients, respectively.
We studied the peculiarities of vaginal microecology in women with AB (Table 4). The atrophic vaginitis, characterized by disappearance of lactobacilli or sharp decline in their titers in the absence of massive colonization by opportunistic microorganisms and the inflammatory component, was revealed in the majority of patients in both groups (32.6% of patients in the main and 36.4% in the control group). The status of “conditional normocenosis”, characterized by decreasing the concentrations of lactobacilli, increasing titers of opportunistic pathogens and by the absence of inflammation, was found with similar frequency (27.9% in the main group and 25.0% in the control group). Bacterial vaginosis were revealed in 14% of patients of the main group and in 9.1% of the patients in the control group. Nonspecific vaginitis, characterized by mild inflammatory response (up to 15 white blood cells per field) and small number of homogeneous microflora, were revealed in 18.6% of patients in the main group and in 22.7% of patients in the control group. Beside that, the vaginal candidiasis was diagnosed in 7% of patients in the main group and in 6.8% of patients in the control group.
Table 3. Relations between levels of НвА1c and development of AB and symptomatic forms of UTI after 12 months
| Indicator | Main group (n = 34) |
Control group (n = 39) |
р |
| Mean НвА1с in the groups | 7.07 ±1.2 | 6.9 ±1.23 | 0.790 |
| No of patients (%) with НвА1с ≥7.5% |
13 (36.1%) | 12 (31.6%) | 0.807 |
| No of patients (%) with AB | 7 (19.4%) | 26 (68.4%) | <0.001 |
| No of patients (%) with UTI | 3 (8.3%) | 7 (18.4%) | <0.001 |
Table 4. Data of vaginal culture tests’ results before and after treatment
| Main group | р | Control group | р | |||
| baseline | after 12 months |
baseline | after 12 months |
|||
| Mean НвА1с % | 8.61 ±2.03 | 7.07 ±1.2 | <0.001 | 8.58 ±1.99 | 6.9 ±1.23 | <0.001 |
| No. of patients (%) with atrophic colitis | 32.6% | 9.1% | <0.001 | 36.4% | 55.3% | ˃0.05 |
| No. of patients (%) with normocenosis | 27.9% | 6.1% | 25.0% | 21.1% | ||
| No. of patients (%) with bacterial vaginosis | 14.0% | 0 | 9.1% | 2.6% | ||
| No. of patients (%) with nonspecific vaginitis | 18.6% | 3.0% | 22.7% | 10.5% | ||
| No. of patients (%) with candidiasis | 7.0% | 6.1% | <0.05 | 6.8% | 7.9% | |
Bacterial composition of the vagina also did not differ in both groups. E. Coli dominated mainly and were found in 71% of patients in the main group and 78% of the patients in the control group.
In our study, special attention was paid to the presence of Lactobacilli, which have protective role of the vagina competing with pathogens whose level is more than 105 CFU / ml and can reach 108–109 CFU/ ml in reproductive age women. Initially Lactobacilli at the amount of >105 CFU/ml were detected in 20 (46.5%) patients in the main group and in 22 (50%) patients in the control group (p >0.05).
After 12 months from the beginning of the treatment, a normal amount of vaginal Lactobacilli was detected in the remaining patients of the main group – 35 (97.2%) – and in 17 (44.7%) patients of the control group (p <0.001).
The vaginal health index (VHI) is used to reveal the severity of atrophic processes in vagina and checked regularly in patients receiving treatment with local forms of hormone therapy. In the main group of patients prior to the treatment it was 2.85, after 12 months it was 4.3 (p < 0.001); in the patients of the control group it remained the same – 2.79 and 2.71 after 12 months, respectively (p >0.05) (Figure 2).
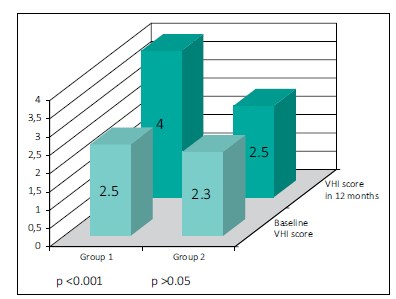
Figure 2. Changes of vaginal culture at baseline and after 12 months.
During the study the nature of the complaints and their severity were analyzed. At the beginning and the end of the study patients were asked to answer the question, whether they notice any unpleasant, disturbing sensation in the vagina. Thus, at the beginning of the study, vaginal dryness was noted in 22 (51.2%), itching of the vulva in 14 (38.6%), dyspareunia in 21 (48.8%) patients of the main group and in 20 (45.5%), 17 (32.6%) and 24 (54.5%) patients of the control group, respectively. After 12 months, in patients of the first group, the frequency of detected signs of atrophic vaginitis decreased: thus, vaginal dryness persisted in two (5.7%) (p <0.001), itching of the vulva in four (11.1%) (p <0, 05), and dyspareunia in six (16.7%) (p >0.05) patients, whereas in patients of the second group, significant changes were not noted: vaginal dryness was found in 19 (50.0%) (p >0.05), itching of the vulva in 18 (47.4%) (p >0.05), and dyspareunia in 17 (44.7%) (p >0.05) patients (Figure 3).
DISCUSSIONS
One of the major non–specific complications in diabetic patients is the urinary tract infection [10]. According to some authors, the frequency of urinary tract infections in patients with diabetes reaches 40%, which is almost three times higher than in the general population [11]. Urinary tract infections often complicate the course of diabetes and associate with a high risk of rapid deterioration of renal function, especially in patients with clinical signs of diabetic nephropathy and arterial hypertension. In our study, during the screening, we diagnosed AB in 22.7% of patients with type II diabetes. Results of our study also showed that in 68.4% of patients of the control group not receiving any treatment, after 12 months of follow–up the AB remained the same, and moreover, in 18.4% of patients in this group, clinical forms of UTI were diagnosed. At the same time, we did not observe a significant difference in the incidence of AB in patients with different levels of HBA1C: AB developed with almost equal frequency in patients with HBA1C both less than 7.5% and greater than 7.5%. Despite that, after 12 months from the start of the study, we observed a significant reduction in the incidence of AB in patients receiving local estriol (group 1). Undoubtedly, proper compensation of diabetes plays a leading role in the prevention and treatment of UTIs. However, giving attention to our results, on can suppose that decompensation of diabetes is not the only cause of AB and clinically evident UTI in postmenopausal women with diabetes.
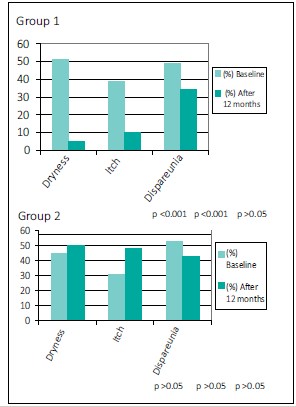
Figure 3. Prevalence of symptoms of atrophic vaginitis at baseline and after 12 months.
Increased frequency of UTI with age in women is associated with the development of significant atrophic changes of the vaginal mucosa and urethra in the postmenopausal period with estrogen deficiency and changes of the vaginal flora. During the objective examination of patients, we have identified changes that are typical for epithelial atrophy associated with estrogen deficiency in postmenopausal women, namely: high pH and low VHI.
Also, our study was undertaken to examine the bacterial state of the vagina in women with AB and diabetes and to clarify the influence of local forms of Estriolon on the vaginal microflora in postmenopausal women with diabetes. According to some authors, the causative agent in the majority of cases of urinary tract infections in patients with diabetes is E.coli, while other less common causes are gram– negative bacteria, staphylococci, and enterococci. [1, 3]. Our results revealed mainly E.coli during vaginal cultural examination and microbiological examination of urine, fully compatible with these procedures.
Treatment with the local forms of estriol led to the restoration of mucosal barrier of the vaginal wall, which was confirmed by an increase of VHI to 4.3, and restoration of vaginal microecology. Based on this, we noted an effective reduction in AB incidence in women of the main group, which in turn reduced the risk of symptomatic forms of UTI.
Despite the high efficiency of the local estriols, after 12 months, seven patients from the main group remained AB and three patients developed clinical forms of UTI. This result is probably due to the fact that in patients with diabetes, population–wide factors contributing to the development of urinary tract infection are combined with specific risk factors inherent in diabetes and its complications: glycosuria, neuropathic bladder, and decreased immune defense.
A small reduction in frequency of AB occurred in the control group. This can be explained by the fact that, according to the study protocol, all women, regardless of whether or not they administered estriol, in case of development of clinical forms of UTI during the study, received antibiotic therapy, and in case of development of nonspecific vaginitis or bacterial vaginosis they receive local intravaginal antibiotic treatment. Thus, the vaginal flora was under constant supervision and, if necessary, corrected, but without use of systemic antibiotic therapy. Such tactics of the patient’s treatment was close to the option of observation, which may also be in actual practice, in case of careful self–attention of woman and understanding the need for regular visits to the doctor. In case, if the vaginal microflora is not tracked, single sanitation of the vagina with subsequent reduction of the titer of bacteria in the urine, may be an intermediate stage and the situation is likely to return to the initial situation, as we have seen in most patients of the control group.
Treatment with estriol also led to significant decrease of dryness and itching of the vagina, which improves the quality of life. The findings on the effectiveness of use of the local forms of estriol are interesting since they expand our understanding of the therapeutic potential of that drug; in addition to the positive impact in case of atrophic vaginitis, the ability to treat AB and therefore, to prevent symptomatic forms of UTI in both postmenopausal patients with diabetes and those in the general population. This preventive approach can become an alternative to the prolonged use of antibiotics.
CONCLUSIONS
Asymptomatic bacteriuria in postmenopausal women with type II diabetes is a risk factor for development of symptomatic UTI. The cause of UTI in postmenopausal women with diabetes is not only decompensated diabetes, but also hormonal changes during menopause. The local forms of estriol are effective in postmenopausal women with diabetes as a treatment of AB and as a prevention of clinically symptomatic urinary tract infections. Therapy with local forms of estriol restores the protective microbial barrier of the vaginal wall, increasing the VHI to values specific to women of reproductive age.
References
- Forland M, Thormas W, Shelokov A. Urinary tract infections in patients with diabetes mellitus: Studies on antibody coating of bacteria. J Am Med Ass. 1977; 238: 1924–1926
- Harding G, Zhanel G, Nicolle L, Cheang M. Antimicrobial treatment in diabetic women with asymptomatic bacteriuria. N Engl J Med. 2002; 347: 1576–1583.
- Zhanel GG,Nicolle LE, Harding GK. Prevalence of asymptomatic bacteriuria and associated host factors in women with diabetes mellitus. The Manitoba Diabetic Urinary Infection Study Group. Clin Infect Dis. 1995; 21: 316–322.
- Geerlings S, Stolk R, Camps M, Netten PM, Collet JT, Schneeberger PM, Hoepelman AI. Consequences of asymptomatic bacteriuria in women with diabetes mellitus. Arch Intern Med. 2001; 161: 1421–1427.
- Balasoiu D, Kessel КС, Kats–Renaud HJ, Collet TJ, Hoepelman AI. Granulocyte function in women with diabetes and asymptomatic bacteriuria. Diabetes Care. 1997; 20: 392–395.
- Stein G, Funfstuck R. Asymptomatic bacteriuria – what to do. Nephrol Dial Transplant. 1999; 14: 1618–1617.
- Merta M, Rysavá R, Tesar V. Urinary tract infection in patients with diabetes mellitus. Vnitr Lek. 2006; 52: 423–425.
- Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, and Hooton TM. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005. 40: 643–654.
- Ooi ST, Frazee LA, Gardner WG. Management of asymptomatic bacteriuria in patients with diabetes mellitus. Ann Pharmacother. 2004; 38: 490–493.
- Geerlings SE, Stolk RP, Camps MJL, Netten PM, Hoekstra JBL, Bouter KP, et al. Prevalence and risk factors for asymptomatic bacteriuria in women with diabetes mellitus. ICAAC 1999; abs 607.
- Kasinath BS, Musais SK, Spargo BH, Katz AI. Non–diabetic renal disease in patients with diabetes mellitus. Am J Med. 1983; 75: 613–617.
Download






