
Complications of mid-urethral slings for treatment of stress urinary incontinence
Article authors




Moscow State University of Medicine and Dentistry, 127206, Vucheticha 21, Moscow, Russia
ABSTRACT
Objective: To compare the incidence of complications associated with the use of retropubic tension-free vaginal tape (TVT) and transobturator tension-free vaginal tape (TVT-O) for the management of stress urinary incontinence (SUI). Methods: In a cross-sectional study, 1081 patients were treated for SUI via mid-urethral slings, and the outcomes of those treated via TVT and those treated via TVT-0 were compared. Patients who suffered from recurrent or mixed urinary incontinence were excluded.
Results: Group 1 included patients treated via TVT (n = 207) and group 2 included those treated with TVT-0 (n = 570). There was a higher incidence of bladder perforation (5.4% versus 0.6%; P = 0.001) and hematoma formation (9.1% versus 1.5%; P = 0.001) in group 1 than in group 2. Compared with group 1, there was higher incidence of vaginal wall perforation in group 2 (0.0% versus 3.8%, P— 0.044). The rate of intraoperative complications was not related to patient age, body mass index, or parity. Of the patients who did not leak urine during a cough test 1 month after surgery, 90.9% still had a negative cough test at the long-term follow-up.
Conclusion: TVT-0 was superior to TVT with regard to the incidence of bladder perforation and hematoma formation, but it resulted in more vaginal wall injuries.
1. Introduction
Surgical treatment for stress urinary incontinence (SUI) has rapidly evolved in the past few decades [1-4]. Retropubic tension-free vaginal tape (TVT) is accepted worldwide as a standard treatment for women suffering SUI; however, serious complications such as bowel injury, major vascular injury, and death can occur with the TVT procedure [5]. Recently, transobturator tension-free vaginal tape (TVT-O) has become more popular because of the similar cure rate and lower complication rate that it promises [3,4,6]. A recent review found that the total incidence of complications ranged from 4.3% to 75.1% for TVT, and from 10.5% to 31.3% for TVT-0 [5]. However, most studies have had a limited number of patients and a relatively short follow-up period [7,8].
The aim of the present study was to evaluate and compare the occurrence of complications associated with the use of TVT and TVT-0 in patients with SUI.
2. Materials and methods
The present cross-sectional study was carried out in the Urology Department of the Moscow State University of Medicine and Dentistry, Moscow, Russia. Between September 1, 2001, and December 31, 2008, 1081 women with SUI underwent surgical treatment for SUI. The type of surgery that the patients underwent was selected on the basis of protocols that were accepted in the institution at the time when the patients were treated. Patients who were allocated to undergo surgery via TVT or TVT-0 were enrolled in the present study. Patients with mixed urinary incontinence or recurrent stress urinary incontinence were excluded from the study. All patients gave full informed consent for participation, and the study was approved by the Ethics Committee of the Moscow State University of Medicine and Dentistry.
Group 1 included patients with pure SUI who underwent surgery with TVT (Ethicon, Somerville, NJ, USA). Group 2 included patients suffering from pure SUI who underwent surgery with TVT-0 (Ethicon). The TVT procedure was carried out as originally described by Ulmsten et al. [2], and the inside-out TVT-0 procedure was carried out as first described by de Leval [4].
For each patient, a detailed history was taken and an in-depth physical examination was done before surgery. The examination included a cough stress test and Bonney test. The following data were also recorded: age at surgery, body mass index (BMI, calculated as weight in kilograms divided by the square of height in meters), menopause status, parity, and number of pregnancies. In addition, a urine culture was tested for each patient.
All procedures were performed by 5 surgeons who were experienced in vaginal surgery. All patients underwent routine clinical examination within 1 month of surgery. Starting in June 2008, patients were contacted again via mail or telephone and, when available, were invited for an additional follow-up visit. At both follow-up visits, patients underwent a thorough physical and vaginal examination, including a cough stress test, uroflowmetry, and postvoid residual urine volume measurement.
Data were analyzed with Statistica 8.0 (StatSoft, Tulsa, OK, USA). Two-tailed Fisher exact tests and Yates-corrected /2 tests were used for statistical analysis. A value of P<0.05 was taken to be significant.
3. Results
Of 1081 patients with SUI, 207 underwent the TVT procedure (group 1) and 570 underwent the TVT-0 procedure (group 2). The flow of patients through the study is shown in Fig. 1. There were no significant differences in patient characteristics between the 2 groups with regard to age at surgery, menopause status, parity, or number of pregnancies (Table 1). There was a between-group difference in BMI, with patients in group 2 having higher a BMI than those in group 1.
The patients experienced various complications (Table 2). Bladder injuries occurred more often when the TVT method was used (5.4% versus 0.6%, P<0.001). All bladder perforations were confirmed by cystoscopy and managed conservatively. Vaginal wall lacerations happened more often when the TVT-0 approach was used (0.0% versus 3.8%, P=0.044). The frequency of other types of complication was similar between patients in the TVT group and those in the TVT-0 group.
We considered that the frequency of intraoperative complications in both groups might be related to patient age, BMI, or obstetric history. Therefore, the characteristics of patients who developed intraoperative complications were compared with those who did not within groups 1 and 2 (Table 3). The frequency of intraoperative complications for both TVT and TVT-0 insertion was not related to patient age, BMI, or parity. Although patients in group 2 (TVT-O) had a higher BMI than those in group 1, there was no significant difference in BMI between group 2 patients who developed intraoperative complications and those who did not (P=0.838).
Table 1 Characteristics of patients in groups 1 and 2.a
Group 1 (TVT) (n = 207)Group 2 (TVT-O) (n = 570)Test P value
Age, years54.1 ±9.355.3 ±9.0t test0.105
BMIb25.3 ±2.926.5 ±4.4t test var. est.<0.001
Parity
0 28 (13.5)69 (12.1)x2 test0.949
1102 (49.3)289 (50.7)
258 (28.0)157 (27.5)
319 (9.2)55 (9.7)
Pregnancy
<458 (28.0)175 (30.7)X2 test0.882
431 (15.0)79 (13.9)
552 (25.1)134 (23.5)
>566 (31.9)182 (31.9)
Postmenopause
No64 (30.9)141 (24.7)Yates-corrected y2 test0.102
Yes 143 (69.1)429 (75.3)
Abbreviations: BMI. body mass index; TVT, retropubic tension-free vaginal tape; TVT-O, transobturator tension-free vaginal tape. a Values are given as mean±SD or number (percentage). b Calculated as weight in kilograms divided by the square of height in meters.
A total of 187 patients in group 1 (90.3%) attended the 1-month follow-up, compared with 537 women in group 2 (94.2%). The cough stress test is one of the tools most commonly used in subjective evaluation of the efficacy of incontinence surgery; however, there is no consensus on the minimal follow-up period that is required before the results of this test become valid. Overall, 377 women who underwent TVT (n = 166; including some patients with mixed incontinence) or TVT-0 (n = 211) were analyzed by cough test within 1 month after the surgery and at longer-term follow-up. There was no significant difference in cough test between patients in group 1 (85.9%) and those in group 2 (84.4%) at the longer follow-up appointment (P = 0.868).
The results showed that 90.9% of patients who had a negative cough test within 1 month of surgery remained dry on a cough test during long-term follow up, whereas 85.2% of patients who leaked urine during the 1-month cough test still had a positive cough test at their long-term follow-up appointment. Only 14.8% of women who leaked urine during their initial cough test ultimately improved (Table 4). Statistical analysis indicated that the results of the 1 -month cough test for patients treated by the TVT method remained the same after the longer follow-up period (P<0.001).
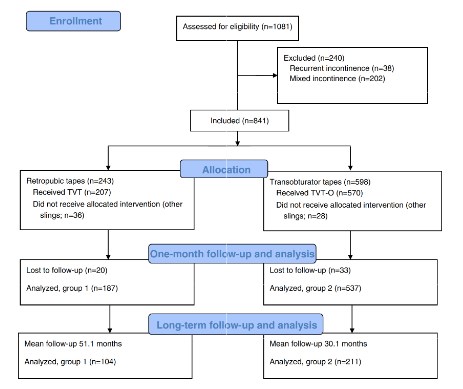
Fig. 1. Flow chart of patients through the study.
Table 2. Complication rates associated with the use of TVT versus TVT-0.a
Group 1 (TVT) (n=187) Group 2 (TVT-O) (n = 537)P valueb
Intraoperative
Hematoma 17 (9.10)8(1.5)0.001
Bladder trauma10 (5.4)3 (0.6)0.001
Postoperative pain4(2.1)11(2.1)0.823
Vaginal laceration015 (3.8)0.044
Postoperative
Tape extrusion 1 (0.5)8(1.5)0.420
De novo overactive bladder 15 (8.0)26 (4.8)0.151
De novo urgency incontinence4(2.1)8(1.5)
0.790
Recurrence16 (8.6)33 (6.2)0.336
Sling incision 4(2.1)3 (0.6)0.142
Post V oid residual urine>100 mL11 (5.9)16 (3.0)0.114
Abbreviations: TVT, retropubic tension-free vaginal tape; TVT-O, transobturator tension-free vaginal tape. a Values are given as number (percentage). b Yates-corrected y2 test.
Table 3. Comparison of patients in groups 1 and 2 who developed intraoperative complications with those who did not.a
Intra-operative complications No complicationsP value
Group 1 (TVT)
Total no of patients 31176
Age53.4 ±9.054.3 ± 9.40.614
BMI 26.2 ±4.725.2 ±2.40.238
Parity
04 (12.9)24 (13.6)1.000
1 18 (58.1)84 (47.7)0.333
25 (16.1)53 (30.1)0.132
3 or more4 (12.9)15 (8.5)0.497
Group 2 (TVT-O)
Total no of patients 37533
Age 54.6 ±8.755.5 ± 9.00.425
BMI 26.6 ±4.026.5 ±4.50.838
Parity
0 6 (16.2)61 (11.4)0.372
116 (43.2)273 (51.2)0.185
210 (27.0)146 (27.4)0.924
3 or more5(13.5)53 (9.9)0.316
Abbreviations: BM1. body mass index (calculated as weight in kilograms divided by the square of height in meters); TVT, retropubic tension-free vaginal tape; TVT-O, transobturator tension-free vaginal tape. a Values are given as number (percentage) or mean±SD. b By t test.
c By 2-tailed Fisher exact test. d By Yates-corrected y2 test.
Table 4. Cough test results of all patients at the 1-month and long-term follow-up appointment
Negative cough test >12 months after surgeryPositive cough test >12 months after surgeryP value b
Negative cough test within 1 month of surgery 318 (90.9)32 (9.1)<0.001
Positive cough test within 1 month of surgery4 (14.8)23 (85.2)-
a Values are given as number (percentage). b By 2-tailed Fisher exact test.
4. Discussion
Tension-free vaginal tape is known to be very effective for the management of female SUI [7,14]. Recent meta-analyses have reported equal cure rates for TVT and TVT-O approaches [8,9].
The stress cough test is a useful and objective test in evaluating the outcome of SUI surgery [9]. It is widely accepted by physicians because it is less time-consuming than the 24-hour pad test, and because it can be easily incorporated into the routine physical examination on follow-up visits. Although the coughing efforts of patients are difficult to standardize, the cough test has been used in a randomized comparative study of TVT and TVT-O [10]. According to the present analysis, the results of a cough test performed within 1 month of surgery has a high probability (90.9%) of remaining the same on prolonged observation.
There is significantly increased risk of bladder perforation and hematoma formation when the tape is inserted via the retropubic route rather than the transobturator route [9]. In the present study, hematomas occurred in 9.1% of patients who underwent the retropubic approach and 1.5% of patients who underwent the transobturator approach. The rate of bladder perforation in the TVT-O group was much lower than that in the TVT group (0.6% versus 5.4%).
Various multicenter randomized controlled trials [11,12] and systematic reviews [8,13] have produced similar results [14-16]. One systematic review found that the occurrence of bladder perforations and pelvic hematomas was significantly less common among patients treated via TVT-O than via TVT [13]. Another review found that the odds of bladder injury (odds ratio 0.13, 95% confidence interval 0.06-0.27) was lower for TVT-O [8].
Vaginal injuries, thigh pain, and groin pain occur more frequently with the TVT-O approach because the tape is passed beneath the pubic bone exits in the groin. According to Meschia et al. [10], groin pain resolved in most patients within 1 month of surgery. Other authors found no significant differences in postoperative pain on the basis of the surgical technique used [12]. In the present study, there was no difference in the occurrence of postoperative pain between the 2 groups.
Tape extrusion usually occurs in the early postoperative period. Unrecognized vaginal perforations or lacerations that occur during TVT-O insertion might lead to subsequent extrusion. Although the occurrence of vaginal wall injury during TVT-O has been found to be very low, the transobturator route is associated with a higher rate of vaginal laceration than the retropubic approach [13]. In the present study, there was significantly higher incidence of vaginal wall injury, mostly in lateral fornix, when the transobturator approach was used (0.0% versus 3.8%, P = 0.044). It is possible that this higher incidence of vaginal laceration was the reason for the slightly higher incidence of mesh extrusion that was observed with the transobturator approach. It is important to note that vaginal wall erosions over the tape are relatively benign and can often be managed with the application of local estrogen.
The incidence of voiding dysfunction was higher in the TVT group, which was expected, as a sling inserted in this manner has a propensity to cause more obstruction than a sling inserted via the ransobturator approach. In the present study, 5.9% of patients in the TVT group and 3.0% in theTVT-0 group (P = 0.114) had residual urine volumes of more than 100 mL on the second day after surgery, which is consistent with other reports [11].
The present study found that de novo urgency incontinence and de novo overactive bladder were present in, respectively, 2.1% and 8.0% of patients in the TVT group, and 1.49% and 4.84% of patients in the TVT-0 group. In general, it is thought that the prevalence of symptoms of voiding dysfunction after sling-based procedures decreases over time.
Increased BMI is a well known risk factor for the development of stress urinary incontinence. One might suppose that overweight patients are not ideal candidates for minimally invasive surgery and have higher intraoperative complication rates than patients with a normal BMI. In the present study, although the patients in group 2 (TVT-O) had a higher BMI than those in group 1, there was no significant difference in BMI among patients who developed intraoperative complications and those who did not in either group.
The main limitations of the present study were the lack of pure randomization, and differences in the timing and number of follow-up appointments between the groups.
In summary, the rate of intraoperative complications for patients treated by the TVT or TVT-0 approach was not related to patient age, BMI, or parity. Bladder perforation and pelvic hematoma formation occurred more frequently when the TVT approach was used. By contrast, the TVT-0 approach was associated with a higher occurrence of vaginal wall injuries. Lastly, the result of the 1-month cough test would seem to be a reliable prognostic factor that is unlikely to change with a longer follow-up period.
Conflict of interest
The authors have no conflicts of interest.
References
- DeLancey JO. Anatomy and biomechanics of genital prolapse. Clin Obstet Gynecol 1993 ;36(4) :897-909.
- Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 1996;7(2):81-6.
- Delorme E. Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol 2001; 11 (6): 1306-13.
- De Leval J. Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol 2003;44(6):724-30.
- Daneshgari F, Kong W, Swartz M. Complications of mid urethral slings: Important outcomes for future clinical trials. J Urol 2008; 180(5): 1890-7.
- Sung VW, Schleinitz MD, Rardin CR, Ward RM, Myers DL. Comparison of retropubic vs. transobturator approach to midurethral slings: a systematic review and meta-analysis. Am J Obstet Gynecol 2007;197(1):3-11.
- Waltregny D, Reul O, Mathantu B. Inside out transobturator vaginal tape for the treatment of female stress urinary incontinence: interim results of a prospective study after a 1-year minimum followup. J Urol 2006;175(6):2191-5.
- Latthe PM, Foon R, Toozs H. Transobturator and retropubic tape procedures in stress urinary incontinence: A systematic review and meta-analysis of effectiveness and complications. BrJ Obstet Gynecol 2007;114(5):522-31.
- Novara G, Ficarra V, Boscolo-Berto R, Secco S, Cavalleri S, Artibani W. Tension-free midurethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials of effectiveness. Eur Urol 2007;52(3):663-78.
- Meschia M, Bertozzi R, Pifarotti P, Baccichet R, Bernasconi F, Guercio E, et al. Peri operative morbidity and early results of a randomized trial comparing TVT and TVT-O. Int Urogynecol J Pelvic Floor Dysfunct 2007;18(14):1257-61.
- Tamussino K, Hanzal E, Kolle D, Tammaa A, Preyer O, Umek W, et al. Transobturator tapes for stress urinary incontinence: Results of the Austrian registry. Am J Obstet Gynecol 2007;197(6):634.el-5.
- Abdel-Fattah M, Ramsay I, Pringle S. Lower urinary tract injuries after transobturator tape insertion by different routes: a large retrospective study. Br J Obstet Gynecol 2006;113(12):1377-81.
- Novara G, Galfano A, Boscolo-Berto R, Secco S, Cavalleri S, Ficarra V, et al. Complication rates of tension-free midurethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials comparing tension-free midurethral tapes to other surgical procedures and different devices. Eur Urol 2008;53(2):288-308.
- Barry C, Lim YN, Muller R, Hitchins S, Corstiaans A, Foote A, et al. A multi-centre, randomised clinical control trial comparing the retropubic (RP) approach versus the transobturator approach (TO) for tension-free, suburethral sling treatment of urodynamic stress incontinence: the TORP study. Int Urogynecol J Pelvic Floor Dysfunct 2008;19(6):171-8.
- Meschia M, Bertozzi R, Pifarotti P, Baccichet R, Bernasconi F, Guercio E, et al. Peri operative morbidity and early results of a randomized trial comparing TVT and TVT-O. Int Urogynecol J Pelvic Floor Dysfunct 2007:18(11 ):1257-61.
- Waltregny D, de Leval J. The TVT-obturator surgical procedure for the treatment of female stress urinary incontinence: a clinical update. Int Urogynecol J 2009;20(3): 337-48.






