
Follow up for urinary continence after pelvic organ prolapse repair
Article authors




Moscow State University of Medicine and Dentistry, Dept. of Urology, Moscow, Russia

Objective:
To evaluate the incidence of stress urinary incontinence (SUI) and anti-incontinence surgery for 6 months in patients after surgical correction of pelvic organ prolapse (POP) by the vaginal approach relative to the preoperative continence status.
Materials and methods:
This study included 82 women suffering from POP (cystocele grade 2-4 by POP-Q) who underwent transvaginal surgical repair. The study was approved by the local ethics committee, and all patients provided signed informed consent. For evaluation of continence, the UDI-6 questionnaire was used. We found that 30 patients (group 1) had concomitant SUI and prolapse. The remaining patients without complaint of SUI were divided into 2 groups: group 2 (n=31) had a negative cough test after prolapse repositioning, and group 3 (n=21) had occult SUI. The results of surgical treatment of POP were evaluated for the presence SUI within 1, 3 and 6 months after the operation during office visits and using the UDI-6 questionnaire.
Results:
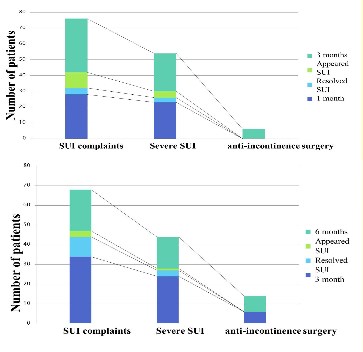
According to the survey performed after 1, 3 and 6 months of follow-up, we obtained the following results (Table 1). No cases of prolapse recurrence were noted during 6 months. At 1 month after surgery, 28 (34% of 82) patients reported the presence of SUI, and 23 (82% of 28) of these patients reported that they were bothered by their condition (according to IIQ-7). The patients remained under observation for six months after surgery to determine the long-term results and further treatment strategy. In total, 34 (41.5%) of 82 patients noted the presence of stress urinary incontinence, and 24 patients (29% of 82, 70% of 34) were strongly disturbed by SUI. However, during the first three months, only 6 patients were re-operated. During the follow-up for the next 3 months (6 months of follow-up), there was a reduction in the complaints related to stress urinary incontinence for 3 patients, and in 7 cases, there was complete resolution of SUI.
Conclusion:
A three-month follow-up period is ideal for the assessment of continence function in patients with severe SUI, and this is the best time to perform anti-stress surgery. In cases with no severe SUI, the follow-up should be continued for up to 6 months or more.
Table 1. Results of follow-up for 6 months.
| 1 month | Dynamics | 3 months | Dynamics | 6 months | |||
| Resolved SUI | Appeared SUI | Resolved SUI | Appeared SUI | ||||
| SUI | 28 (34%) | 4 | 10 | 34 (41%) | 10 | 3 | 21 (27%) |
| Severe SUI | 23 (28%) | 3 | 4 | 24 (29%) | 3 | 1 | 16 |
| Number of re-operated patients | 0 | 6 | 8 | ||||
Acknowledgement:
The study was funded by the grant of The Ministry of Education and Science, project 14.132.21.1784






