
MALE LOWER URINARY TRACT SYMPTOMS: IS THERE ANY BREAKING NEWS?
Article authors

ABSTRACT
During recent decades, the lower urinary tract symptoms (LUTS) presented by patients have remained the same, but our understanding and treatment options have improved due to progressions in the field of functional urology. The role of nitric oxide in the ageing of the pelvic floor, bladder, prostate, and urethra is an important mechanism of LUTS. Phosphodiesterase-5 inhibitors are increasingly used in the treatment of these patients. Metabolic syndrome has been suggested as another important aetiological factor for both storage and voiding symptoms. Despite dramatic evolution in treatment strategies, non-adherence to pharmacological therapy is very high. The ineffectiveness and side effects are the primary reasons for the patients stopping treatment. The different aspects of combination therapy and the reported outcomes of patients will be discussed in this review.
INTRODUCTION
The term lower urinary tract symptoms (LUTS) includes many medical problems in male urology and represents one of the most common clinical complaints in adult men. It can be divided into storage, voiding, and post-micturition symptoms. In the past, male LUTS was attributed to prostatic diseases and conditions; this was the case even for male storage symptoms. In 1997, Drs. Abrams and Wein introduced the term of overactive bladder (OAB) when they co-chaired a consensus conference.1 Furthermore, increasing knowledge of the role of bladder dysfunction in LUTS pathophysiology has dramatically changed the landscape of the treatment options for both males and females. The LUTS presented by patients remain the same, but our understanding and treatment options have improved as we have progressed in the field of functional urology. LUTS are not necessarily the same group of diseases in each patient, but rather a complex of similar complaints that are created by one or many diseases (Figure 1). Moreover, many patients with LUTS present with more than one of the factors involved.
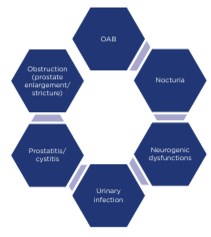
Figure 1: Main causes of male lower urinary tract symptoms (LUTS). OAB: overactive bladder.
The multifactorial aetiology of LUTS forces us to regard the whole urinary tract as a single functional unit. This review presents recent developments and updates in LUTS.
PELVIC FLOOR AGEING
The pathophysiology of LUTS in men is still far from being fully explored. Recent investigations in this field demonstrated the role of pelvic ischaemia, caused by RhoA/Rho-kinase pathway activation. Autonomic overactivity and increased afferent neural activity of the bladder are caused by highly complex and multifactorial factors. The role of nitric oxide in the relaxing of the smooth muscles of the bladder, prostate, and urethra is far from being completely understood. All of these important mechanisms of benign prostatic hyperplasia (BPH)/LUTS may be positively affected by phosphodiesterase-5 (PDE5) inhibitors.
Nitric oxide synthase (NOS) was recently introduced as another pathogenic mechanism that plays a role in bladder outlet obstruction (BOO) and LUTS in men. During the last century, PDE5 inhibitors have been increasingly used in the treatment of male LUTS. A recent study of PDE5 distribution in human tissues demonstrated that PDE5 activity in the bladder, prostatic urethra, and prostate tissues is distributed unevenly, with less in the bladder neck, more in prostatic urethra, and even more in prostate tissue.2 This selective distribution and activity of PDE5 in patients suffering from LUTS, and a decrease of the RhoA/Rho-kinase contractile mechanism in the bladder, could be the simplified rationale for the use of PDE5 inhibitors to diminish bladder dysfunction and outlet obstruction. The role of the bladder as a target of PDE5 inhibitors in LUTS is further explored by the functional improvement of urodynamic parameters in spinal cord injury patients after PDE5 inhibitor administration3 and the effectiveness of PDE5 inhibitors on continence recovery after radical prostatectomy a prostate cancer, and therefore in men without a prostate.4 Chronic ischaemia due to pelvic artery insufficiency that is caused by metabolic syndrome induces morphologic and functional changes in the bladder and prostate.5 Additionally, modulation of autonomic nervous system overactivity and bladder/prostate afferent nerve activity by PDE5 inhibitors has also been suggested.5 Although the exact mechanism of these medications still needs to be clarified, inhibition of PDE5 that increases the amount of NO in the smooth muscles has been shown to have an effect on several pathogenetic pathways contributing to LUTS.
METABOLIC SYNDROME AND LOWER URINARY TRACT SYMPTOMS
BPH and OAB may be aetiologically linked, not only in a cause-and-effect way but also by shared risk factors. As mentioned above, bladder ischaemia and metabolic syndrome have been suggested as aetiological factors for both storage and voiding disorders in LUTS. Epidemiologic studies suggest that metabolic syndrome components, such as increased waist circumference, are associated with the severity of LUTS as assessed by the international prostate symptom score (IPSS).6 The proposed mechanism behind this observation is hyperinsulinaemia-associated increased sympathetic activity, leading to increases in smooth muscle contraction throughout male genitourinary tract structures, and subsequently LUTS. Other proposed mechanisms include impaired nitrergic innervation, increased Rho kinase activity, proinflammatory status, and changes in sex hormones. Mild-to-moderate bladder ischaemia occurring in metabolic syndrome damages the urothelium and intramural nerves, and induces detrusor overactivity (DO), resulting in the appearance of OAB. This was also proved in an animal study of rabbits with hyperlipidaemia and progressive atherosclerosis, where a reduction in bladder blood flow was associated with DO and urinary frequency.7 Nevertheless, other studies refute the association of OAB and metabolic syndrome.8
The influence of testosterone and oestradiol on LUTS in men with BPH is another hot topic. In a recent, post-hoc analysis of 958 men with a history of LUTS of >6 months and an IPSS ≥13, patients were randomised to 5 mg tadalafil daily.9 The aims of the investigation were to observe the characteristic testosterone levels in these patients, and to evaluate the cross-sectional relationship of 17β-ostradiol, testosterone, and LUTS before treatment. At the same time, a longitudinal association between baseline 17β-ostradiol, testosterone, and any improvement or worsening of LUTS after 12 months of tadalafil treatment was carefully analysed. According to the published data, the baseline testosterone was not significantly associated with IPSS score, whilst 17β-ostradiol was inversely correlated with IPSS. The PDE5 inhibitor tadalafil was more effective in patients with lower baseline levels of 17β-ostradiol. The increase in the IPSS level was more visible with total voiding scores than in storage domains. It was shown that lower levels of testosterone were not predictive of change in IPSS after tadalafil treatment. However, men with lower 17β-ostradiol levels demonstrated a better response to treatment.
COMBINATION THERAPY
The coexistence of storage and voiding symptoms in men poses a significant therapeutic challenge. There are quite a few agents to use either alone or in combination to target the prostate or the bladder. If the exact aetiologic factors and mechanisms for male LUTS were known, patient selection for certain treatments and, most importantly, treatment selection for individual patients would be much easier. Unfortunately, the pathophysiology of male LUTS remains to a certain degree an enigma, despite advances in our understanding of the mechanisms involved and a continuous effort to decode relevant molecular pathways.10 For many years, BOO was aetiologically linked to all male LUTS and therefore reduction of the dynamic and mechanical components of BOO, with alpha-blockers (AB) and 5-alpha-reductase inhibitors (5ARIs) respectively, was the primary therapeutic target.11 Storage symptoms were either ignored or expected to improve once their cause, outlet obstruction, was relieved. This belief was based on evidence that urethral obstruction causes both morphological and functional changes in the bladder that are responsible for the storage symptoms. Failure to substantially relieve storage symptoms with prostate-targeting therapies led to an increasing recognition of the bladder as a major contributor to male LUTS. Regardless of whether DO was the consequence of obstruction or a distinct pathology, it had to be treated. The addition of antimuscarinics for residual storage symptoms was initially used reluctantly, due to fear of retention. Nevertheless, current knowledge suggests that antimuscarinics as an add-on treatment, as well as part of combination regimens for treatment initiation, do not substantially increase the risk of retention, at least for patients with moderate outlet obstruction and residual volumes < 150–200 mL. For patients with more severe obstruction and larger residual storage symptoms, the risk is not adequately assessed, and caution is advised.
Traditionally, AB and antimuscarinics were the first-line medications for patients with LUTS.12 Nonadherence to this pharmacological therapy is very high. The ineffectiveness and side effects are often cited as the primary reasons for patients stopping the treatments. Patient adherence to the medication and the clinical consequences of non-adherence were analysed in men with BPH-associated LUTS; the study was looking at the differences between drug classes whilst comparing mono versus combination therapy. A large retrospective cohort study using an administrative database of 1.5 million Italian men was carefully analysed. Patients >40 years of age, prescribed AB and 5ARIs, alone or in combination (AB/5ARI) for BPH-associated LUTS were investigated. The 1-year and long-term adherence were examined, together with the analysis of the rate of hospitalisation for BPH-related surgery.13
Patients exposed to at least 6 months of therapy had a 1-year overall adherence of 29% (AB: 35%; 5ARI: 18%; AB/5ARI: 9%). Patient adherence progressively decreases to 15%, 8%, and 3% for AB, 5ARI, and AB/5ARI, respectively, in the 5th year of follow-up. Patients on the combination therapy had a higher discontinuation rate than others. At the same time, AB/5ARI was associated with a reduced risk of hospitalisation for BPHrelated surgery compared with AB. In general, the adherence to therapy for BPH-associated LUTS is low but varies depending on drug group. Patients under combination therapy have a higher treatment discontinuation rate for reasons that should be investigated further in the future. It is obvious that new strategies aiming to increase patient adherence to the prescribed treatment are necessary to prevent BPH progression.
QUALITY OF LIFE
Storage symptoms, the most common and bothersome subset of LUTS, predominantly affect the aged population with a worldwide distribution. Traditionally, nocturia is described as the most troublesome symptom in males with LUTS. A recent Japanese study14 investigated the impact of storage symptoms on health-related quality of life (QoL) in male patients. Overall, 567 men who presented in a urology department completed the IPSS, incontinence-frequency score (IFS), and 36-Item Short-Form Health Survey (SF-36) questionnaires. Among 230 men with urological symptoms, it was shown that IPSS item scores of urgency, nocturia, and straining correlated with scores of the SF-36.
Incontinence was counted as the most influential factor that had a negative impact on general health perception, physical activities, vitality, social functioning, and mental health. Nocturia, straining, and urgency were significantly associated with a negative impact on QoL.
The relationship between LUTS, depression, and anxiety in men remains unclear. Pelvic inflammation is an independent risk factor for LUTS and depression according to up-to-date knowledge. An interplay between depression and LUTS accompanied by inflammation was investigated in a trial using patients randomly included from an urban community-dwelling cohort of men aged 35–80 years at recruitment (n=1195; sample response rate: 67.8%). Among 730 men who attended baseline (2002–5) and follow-up clinic visits (2007–10) without prostate or bladder cancer and the history of surgery, antipsychotic medication use, or neurodegenerative conditions were included in the present study. The incident of storage and voiding LUTS and the incidence of depression and anxiety were adjusted to serum inflammatory markers (high-sensitive C-reactive protein, tumour necrosis factor-alpha, interleukin-6, myeloperoxidase, soluble E-selectin). Multiple regression analysis was used to assess the moderating effect of all factors.15
Men with storage LUTS and anxiety at baseline had an increased likelihood of depression. Otherwise, men with depression and voiding LUTS were more likely to have anxiety at follow-up. Inflammation markers presented a significant moderating effect on the development of storage LUTS, depression, and anxiety. Finally, the authors conclude that there is a bidirectional relationship between storage LUTS and both depression and anxiety.
CONCLUSION
Ageing of the pelvis with ischaemia of the pelvic organs is being actively investigated. Within the frames of this concept, PDE5 inhibitors are becoming pathogenic treatment options for LUTS, as well as for conditions related to the bladder and prostate. Metabolic changes and hypogonadism are playing an important role in the symptom intensity and the efficacy of the medications. In spite of significant efforts, the adherence of the patients to the different LUTS treatments remain insufficient for all pharmacological groups and combinations. The QoL of the patients with LUTS is significantly diminished by nocturia, urgency, and straining, often causing depression and anxiety. Further investigations are ongoing into both the pathophysiology and pharmacogenetics of these complex patients.
Keywords: Lower urinary tract symptoms (LUTS), benign prostatic hyperplasia (BPH), overactive bladder (OAB), incontinence.
REFERENCES
1. Abrams P, Wein AJ. Introduction: overactive bladder and its treatments. Urology. 2000;55(5, Supplement 1):1-2.
2. Andersson KE et al. Chronic Pelvic Ischemia: Contribution to the Pathogenesis of Lower Urinary Tract Symptoms (LUTS): A New Target for Pharmacological Treatment? Low Urin Tract Symptoms. 2015;7(1):1-8.
3. Gacci M et al. Vardenafil improves urodynamic parameters in men with spinal cord injury: results from a single dose, pilot study. J Urol. 2007;178(5):2040-3.
4. Patel HR et al. Effects of tadalafil treatment after bilateral nerve-sparing radical prostatectomy: quality of life, psychosocial outcomes, and treatment satisfaction results from a randomized, placebo-controlled phase IV study. BMC Urology. 2015;15:31.
5. Morelli A et al. Acute vardenafil administration improves bladder oxygenation in spontaneously hypertensive rats. J Sex Med. 2010;7(1): 107-20.
6. Lee RK et al. Central obesity as measured by waist circumference is predictive of severity of lower urinary tract symptoms. BJU Int. 2012;110(4): 540-5.
7. Yoshida M et al. The effects of chronic hyperlipidemia on bladder function in myocardial infarction-prone Watanabe heritable hyperlipidemic (WHHLMI) rabbits. Neurourol Urodyn. 2010;29(7):1350-4.
8. Behr-Roussel D et al. Vardenafil decreases bladder afferent nerve activity in unanesthetized, decerebrate, spinal cord-injured rats. Eur Urol. 2011;59(6): 272-9.
9. Egan KB et al. Do baseline estrogen and testosterone affect lower urinary tract symptoms (LUTS) prior to or after pharmacologic treatment with tadalafil? Andrology. 2015;3(6):1165-72.
10. Al-Zahrani AA, Gajewski JB. Association of symptoms with urodynamic findings in men with overactive bladder syndrome. BJU Int. 2012;110(11 Pt C):E891-5.
11. Kaplan SA et al. Combination therapy with doxazosin and finasteride for benign prostatic hyperplasia in patients with lower urinary tract symptoms and a baseline total prostate volume of 25 Ml or greater. J Urol. 2006;175(1):217-20.
12. Drake MJ et al. Long-term safety and efficacy of single-tablet combinations of solifenacin and tamsulosin oral controlled absorption system in men with storage and voiding lower urinary tract symptoms: results from the NEPTUNE Study and NEPTUNE II open-label extension. Eur Urol. 2015;67(2):262-70.
13 Cindolo L et al. Patient’s adherence on pharmacological therapy for benign prostatic hyperplasia (BPH)-associated lower urinary tract symptoms (LUTS) is different: is combination therapy better than monotherapy? BMC Urol. 2015; 15(1):96.
14. Okada T et al. [The impact of lower urinary tract symptoms on generic healthrelated quality of life in male patients without co-morbidity]. Nihon Hinyokika Gakkai Zasshi. 2015;106(3):172-7.
15. Martin S et al. Lower Urinary Tract Symptoms, Depression, Anxiety and Systemic Inflammatory Factors in Men: A Population-Based Cohort Study. 2015; 10(10):e0137903.






