
Mesh–related and intraoperative complications of pelvic organ prolapse repair
Article authors





1Urology Department of Moscow State University of Medicine and Dentistry, Moscow, Russia
2Moscow Regional Institution of Obstetrics and Gynecology, Moscow, Russia
Introduction To evaluate the rates of complications of pelvic organ prolapse repair and to determine their risk factors.
Material and methods The study included 677 patients operated for pelvic organ prolapse with trocar guided Prolift mesh. Patients were followed up within 1 and 3 months. A phone interview was conducted and patients with complaints were invited and evaluated in office settings.
Results Mean age was 60 years. For the phone interview, 86.5% of patients were available. Overall complication rates were 22.5% (152/677). Fifteen patients (2.2%) developed bleeding over 500 cc; pelvic hematomas – 5.5%; perineal hematomas – 2.5%; urethral injuries – 0.3%; bladder injury in 1.6%; rectal damage in 0.7% and ureteral trauma in 0.2%.
Mesh related complications included: erosions in 4.8%; vaginal synechiae – 0.3%; protrusion of mesh into the bladder – 0.15%; vesicovaginal fistula with mesh protrusion – 0.3%; mesh shrinkage – 1%; dyspareunia and pain in 2.4% cases. Pelvic abscess was found in 0.6% including one case of lethal necrotizing fasciitis. The risk factors of complications were assessed via logistic regression analysis.
Conclusions Younger age, less prominent prolapse, hematomas and concomitant hysterectomies are associated with higher risk of complications.
Key Words: pelvic organ prolapse, complications, mesh related, risk factors
INTRODUCTION
At the present time, synthetic meshes are frequently used in pelvic organ prolapse (POP) surgery with very good clinical outcomes. At the same time, there has been an increase in the number of mesh–associated complications. Although rare, these complications can have serious consequences. During the past several years, many reports of complications associated with synthetic meshes have been published in the literature. The most frequent complications include vaginal mucosa erosion, mesh shrinkage, infections, pain, urinary tract disorders and a recurrence of prolapse. There have also been reports of rare complications, such as bowel, bladder, and blood vessel perforation during insertion.
The recent randomized controlled trial published by Altman et al. showed improved anatomical and functional outcomes following an anterior transvaginal mesh (TVM) procedure compared to native tissue repair [1]. Over the years, the transvaginal mesh kit has become a widespread treatment option in POP and has been entered in routine practice in majority pelvic floor surgery centers worldwide [2, 3]. This situation enhances the risk of complications, which can sometimes be very severe. Furthermore, when complications occur, the lack of knowledge and experience can cause a further severe morbidity if it is not diagnosed and treated in a proper way [4–7].
It is known that using mesh is associated with high rates of complications and repeat operations in genital surgery [8, 9]. A systematic review by Diwadkar et al. [10] showed that women in the mesh kit group had a higher re–operation rate than those who had a traditional surgery or sacrocolpopexy. Different re– interventions were done due to complications including mesh protrusion (5.8 %), pain (2.5%) and dyspareunia (2.2%). Marcus–Braun and von Theobald [11] described 104 surgeries in 83 women who had complications of previous mesh surgery. The indications for the re–interventions included mesh protrusion, infection, pain, granuloma, voiding problems and mesh shrinkage. Altman et al. [1] also reported more complications in the group of women who had undergone mesh repair. This included more bladder injury (3.5%), pelvic pain (2.5%) and mesh exposure (3.2%). Complications of vaginal mesh are often overestimated, sometimes overemphasized and often poorly described and managed. The aim of our study was to assess the complications, to determine the way of prevention and treatment of complications following vaginal mesh surgery interventions. The serious complications encountered are discussed in detail.
MATERIAL AND METHODS
This is a retrospective, multicenter study conducted in 7 referral pelvic floor repair centers. Local Ethics committees approved the protocol of the study. Inclusion criteria for the study were patients operated for pelvic organ prolapse with vaginal meshes. The surgical procedure was standardized, according to local protocols, and limited to using a trocar–guided transvaginal mesh kit (Prolift, Gynecare, USA) for repair of anterior, posterior and apical vaginal prolapse.
We have retrospectively analyzed the intraoperative and early postoperative complication rates for these patients by reviewing patients’ files. According to the local practice, follow–up visits at 1 and 3 months were done for the patients. This data was extracted and analyzed as well.
At the start of the study, a phone interview was conducted in order to evaluate the patients self–perception. All patients who considered themselves symptomatic were invited for thorough office check–up that included vaginal exam, uroflowmetry and postvoid residual measurement followed by cystoscopy when appropriate.
The analysis was done using Statistica 6.0 software. The baseline characteristics are presented using absolute and relative ratio with either means or standard deviations (SD). Comparisons of patient proportions were presented as odds ratio (OR) with 95% confidence intervals (CIs). P values < 0.05 were considered statistically significant for all comparisons.
RESULTS
In total, 677 cases using mesh devices were analyzed from a period between 2006 to 2010. Overall, 303 patients have had anterior repair, 51 posterior repair, 232 vaginal vault repair and 91 patients had combined anterior and posterior surgery. Only 86.5% (586/677) were available for phone interview, others were lost for follow–up due mainly to failure to contact the patients.
During comparative data analysis all patients were divided into two groups. Group 1 included 525 women without complications after mesh surgery with mean age of 60 (±12.7) years. Group 2 included 22.5% of patients (152/677) who have had any kind of complications, including intra–operative and mesh–related injuries. These complications are comprehensively presented in Table 1.
Intraoperative and early postoperative complications were registered in 88 patients (12.9%).
Bleeding
The most common injuries were related to bleeding and were limited to pelvic/perineal hematomas and severe intraoperative blood loss (more than 500 cc). Fifteen women (2.2%) had blood loss over 500 ml, although three of these women were associated with vaginal hysterectomies. Three women had serious vascular injuries: inferior gluteal vessels, obturator vessels, paraurethral venous plexus. In all these cases, blood transfusion was done due to the massive blood loss. Main symptoms of vaginal, retropubic or perineal hematomas in the postoperative period were fever, significant decrease in the level of hemoglobin, buttock pain and urinary retention due to compression of bladder neck. Moreover, ten major vaginal hematomas (>500 ml) led to urinary retention or transformed into an abscess. Several of them required a transcutaneous drainage. Subdermal, perineal and buttock hematomas were solved without any additional interventional therapy.
Table 1. Complications of POP repair with mesh prosthesis
| Complications | % (N) 22.5% (152) |
| Intraoperative and early postoperative | |
| Vaginal/pelvic hematomas | 5.5% (37) |
| Perineal hematomas | 2.5% (17) |
| Bleeding more than 500 cc | 2.2% (15) |
| Bladder injuries | 1.6% (11) |
| Rectal damage | 0.7% (5) |
| Urethral traumas | 0.3% (2) |
| Ureteral trauma | 0.15% (1) |
| Mesh related | |
| Mesh erosions | 4.8% (32) |
| Pain and dyspareunia | 2.4% (16) |
| Mesh shrinkage | 1% (7) |
| Pelvic abscess | 0.6% (4) |
| Symptomatic vaginal synechiae | 0.3% (2) |
| Protrusion into the bladder | 0.15% (1) |
| Fistulas with mesh | 0.3% (2) |
Urinary tract injuries
The second most common type of complication was urinary tract damage. Bladder, urethral and even ureteral injuries occurred during dissection of the tissues, insertion of trocars of anterior mesh device, and fixation of the mesh to the bladder neck. All but two cases of urinary tract injuries were intraoperatively found on cystoscopy at the time of surgery. In one of the overlooked cases it led to stone formation after protrusion of the mesh into the bladder. Another undetected bladder injury was confirmed on the 7th day after surgery when continuing hematuria increased. Cystoscopic view confirmed bladder damage with mesh. Undetected bladder injury led to stone formation and later transformed to protrusion of the tape into the bladder in one case. That patient required laparotomy and removal of the mesh with resection of the bladder wall.
Ureteral trauma
A single case of ureteral injury happened to a 70– year–old woman with stage III cystocele who underwent anterior transvaginal mesh implantation of a four–armed anterior implant. It was inserted using four trocars passed through the obturator foramina. At the second day post–surgery, the patient noted moderate edema and pain in her right hip. Her temperature was 37.2°C, and the blood tests revealed normal white and red blood cell counts. A contrast CT scan showed urinary leakage on the right side (Figure 1) extending to the interfascial space of the right hip. A retroperitoneal approach revealed complete injury of the right ureter at the level of the right posterior arm of the mesh. Ureteroneocystostomy was performed.
Rectal injuries
Five cases of rectal injuries occurred during the initial dissection of the rectum from the posterior vaginal wall due to presence of extensive scar tissue and therefore they were not related to mesh insertion. In three cases the injury was repaired before insertion of the mesh with no further postoperative complications. In all cases the mesh was not inserted and traditional posterior colporrhaphy was done. None of the cases required colostomy.
Mesh–related complications
Mesh–related complications were registered in 64 cases (9.4%) and they included vaginal adhesions in 2 (0.3%) women, vaginal extrusions in 32 (4.8%), bladder erosion in 1 (0.2%), urethro–vaginal fistula in 2 (0.3%), mesh–shrinkage in 7 (1%), buttock and perineal pain in 16 (2.2%), mesh–infection in 4 (0.6%).
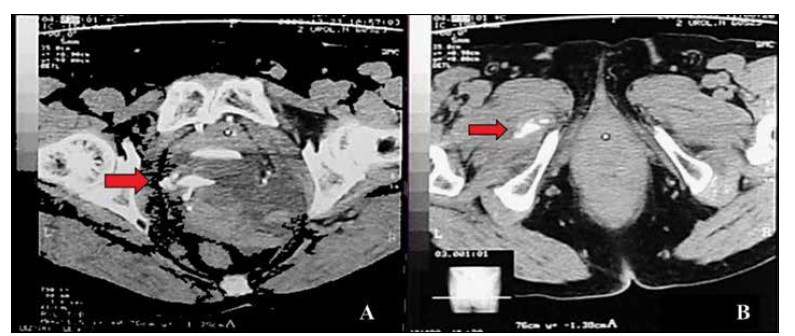
Figure 1. CT scan showing urinary leakage on the right side (A). Urine leakage extending to the interfascial space of the right hip (B).
Mesh extrusions
Extrusions are the most common mesh–related complications. All vaginal mucosa erosions with protrusion of the mesh were detected on vaginal examination between 2 and 24 weeks after surgery. All women with mesh extrusions had symptoms of offensive vaginal discharge and dyspareunia. In 20 (12%) women with vaginal protrusion of the mesh, concomitant vaginal hysterectomy was undertaken. The rate of mesh protrusion among those without hysterectomy was 2.4%.
In general, some vaginal extrusions were less than 0.5 cm in size (18 cases) and were managed conservatively with local estrogens, afterwards they all required partial excision of exposed mesh. Three women had persistent mesh extrusions requiring secondary mesh excision.
Infections/Necrotizing fasciitis
Two women had large mesh extrusions with signs of local infections and buttock phlegmonal abscess following anterior and posterior mesh implantation. Patients were treated by total surgical removal of the mesh, under general anesthesia.
Moreover, we have registered a case of necrotizing fasciitis in a patient with stage III POP. She had a history of intrauterine device (IUD) inserted 30 years ago. Uterine ultrasound proved the presence of IUD and showed no hyperplasia of the endometria. The patient opted for vaginal hysterectomy and prolapse repair with mesh kit (Prolift Anterior, Gynecare). Morphological examination proved the presence of IUD and found an endometrial cancer (T1N0M0). At day 6 after the surgery, the patient developed swelling and redness on the thighs, severe pain, high fever, hypotension and other signs of systemic toxicity. Physical exam showed pigmentation in medial parts of both thighs with crepitation. Necrotizing fasciitis of both thighs was diagnosed. The patient was emergently taken to the surgical theater for fasciotomy and debridement. Non–clostridial Streptococci were identified from the wound. After the surgery, the patient was treated in an intensive care unit for 18 days and afterwards she died due to intoxication and fatal coagulopathy [12].
Mesh shrinkage
Shrinkage of synthetic mesh after implantation is one of the most serious complications. It was registered in 5 cases in our study and was characterized by severe vaginal pain, dyspareunia, vaginal shortening, urethral obstruction, and prolapse recurrence. Surgical intervention is often required to alleviate symptoms. It involves mobilization of the mesh, dividing of the fixation arms, and excision of contracted mesh. The surgical intervention is potentially associated with an increased risk of visceral injury and hemorrhage. Tissues are often firmly adhered to the mesh and surgical planes are often unknown. The goal of surgical management is to relieve the tension by dividing the central graft from the arms and excising all areas of contracted mesh.
Risk factors for complications
Statistical analysis of the data revealed several risk factors associated with intraoperative, early postoperative and mesh related complications. The patients younger than 55 years have 3.3 times more chance to develop perioperative complications. The risk for mesh related complications is even higher and amounted to 8.2, but this finding was compromised by a wide confidence interval that had made it statistically non–significant.
Concomitant vaginal hysterectomy 2.8 times increases the risk of surgical complications and 2.4 times for mesh–related ones. Development of postoperative hematomas increases the risk of mesh–related complications by 2.5 times. According to our data, patients with less prominent prolapse (< III POP–Q) repaired by mesh have had 4 times more risk for mesh related problems. Other factors such as BMI, high stage prolapse and others listed in Table 2 do not influence the risk of complications.
DISCUSSION
Modern surgical techniques for the management of pelvic organ prolapse are presumed to be a minimally invasive with almost no complications. At the same time, it should be emphasized that the implantation of surgical mesh is permanent, that some complications associated with the implanted mesh may require additional surgery, and that even surgery may not correct the complication.
Small vessel injuries during extensive dissection, especially of paravesical and pararectal spaces were hardly avoidable. The blind insertion of the trocars into the obturator foramen, ischiorectal fossa, ileococcygeus muscle and the sacrospinous ligament exposes the patient to the potential injury to the rectum, bladder, inferior gluteal vessels, pudendal nerve and vessels, and the sciatic nerve. That is why the absolute safety of transobturator access raises a lot of doubts. Anatomical landmarks are essential in pelvic organ prolapse repair. During hands–on training for mesh surgeries, it is necessary to pay special attention to safety landmarks and anatomical topography. The ureters are always in close proximity to the cervix, and ureteral injury should be considered as a potential risk in patients with extensive prolapse.
Despite the risk of mesh extrusion, which is a specific complication of using any graft, synthetic materials are preferred over autologous graft materials because synthetic graft materials are durable, largely available and relatively inexpensive [13]. Synthetic graft materials also reduce the risk of morbidity and operative time as fascia is not harvested. Mesh exposure can be caused by the use of any type of synthetic graft material. It is not possible to identify the precise rate of mesh exposure due to a lack of long–term follow–up; however, the overall rate based on short–term follow–up has been reported to be 0.8–16% [14, 15]. Polypropylene mesh is the preferred synthetic graft material because of the lower mesh exposure rate [15]. In addition to mesh type, other factors, such as surgical technique, concomitant hysterectomy, cigarette smoking, hormonal status and a history of medical diseases, may be related to mesh exposure. According to the present data there are differences in the rates of mesh extrusions with different materials: 7.5% for braided polyester, 5.1% for polypropylene, 9.1% for porcine dermis, 0% for expanded polytetrafluoroethylene (ePTFE), 25% for ePTFE plus synthetic graft and 19% for any ePTFE [15].
Concomitant hysterectomy has been evaluated in a number of mesh exposure related studies and inconsistent findings have been obtained. Another study in which laparoscopic ASC was performed showed that previous or concurrent hysterectomy did not affect mesh exposure [16]. Densinger [17] compared total abdominal and supracervical hysterectomy groups in patients undergoing ASC and determined that mesh exposure was increased sevenfold (95% CI, 2.3–19.6%) in the group in which total abdominal hysterectomies were performed. In our study, a 2.8–fold increase in mesh exposure was observed in the concurrent hysterectomy group compared to the previous hysterectomy group. In our opinion, there is more than one factor involved in mesh exposure.
This large retrospective cohort study included 677 patients suffering with pelvic organ prolapse and operated with trocar guided mesh kits. We have found that 22.5% of patients presented with any type of complication, either perioperative or mesh related. The retrospective design was the main limitation of the study, besides the fact that mesh related complications were investigated only in those cases when the patients were symptomatic. Some patients were lost for follow–up (23.5%). With a cross sectional evaluation of the patients, the rate of asymptomatic complications, such as mesh extrusions or mesh shrinkage might become more prominent.
Nevertheless, trocar guided mesh repair of the POP might be a cause of serious complications, that may become even life threatening. Further studies with objective evaluation and long term follow–up of the patients are urged in the nearest future.
Table 2. Risk factors and complications following vaginal mesh surgery
| Risk Factors | Operative complications | Mesh–related complications | ||
| OR | 95%CI | OR | 95%CI | |
| Age <55 years | 3.32 | 2.2–05* | 8.2 | 2.5–14.9*** |
| BMI >35 | 1.2 | 0.8–1.7** | 0.3 | 0.2–1.8** |
| Endocrine diseases | 0.6 | 0.5–1.2** | 1.2 | 0.5–2.4** |
| Genitourinary disease | 0.7 | 0.5–1** | 1.3 | 0.7–2.4** |
| POPQ II st. | 2 | 0.9–4.5** | 4 | 1.7–8.9* |
| POPQ IV st. | 2 | 1–4** | 3 | 1.5–6* |
| Total operating time >120 min |
10 | 5.4–18.2*** | 6 | 1.2–10.9*** |
| Vaginal hysterectomy | 2.8 | 1.7–4.6* | 2.4 | 1.3–4.4* |
| Postoperative hematomas | - | - | 2.5 | 1.4–5.1* |
*statistically significant; **statistically non–significant; ***statistically non–significant because of large variance of CI
CONCLUSIONS
Mesh surgery for pelvic organ prolapse has been tremendously reviewed during the last years. Taking this into consideration, a thorough evaluation of mesh related complications is very important for proper planning of surgery and developing informed consent. According to our study we have found that younger age, less prominent prolapse and concomitant hysterectomies are associated with a higher risk of peri–operative and mesh–related complications. The development of postoperative hematomas increases the risk of mesh–related complications.
References
- Falconer C (2011) Anterior colplorrhaphy versus transvaginal mesh for pelvic organ prolapse. N Engl J Med. 2011; 364: 1826–1836.
- Hurtado EA, Appell RA Management of complications arising from transvaginal mesh kit procedures: a tertiary referral center's experience. Int Urogynecol J Pelvic Floor Dysfunct. 2009; 20: 11–17.
- Bako A, Dhar R. Review of synthetic mesh–related complications in pelvic floor reconstructive surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2009; 20: 103–111.
- Abdel–Fattah M, Ramsay I. Retrospective multicentre study of the new minimally invasive mesh repair devices for pelvic organ prolapse. BJOG. 2008; 115: 22–30.
- Jacquetin B, Cosson M. Complications of vaginal mesh: our experience. Int Urogynecol J. 2009; 20: 893–896.
- Lowman JK, Jones LA,Woodman PJ, HaleDS. Does the Prolift system cause dyspareunia? Am J Obstet Gynecol. 2008; 199: 707e1–707e6.
- Altman D, Elmer C, Kiilholma P, Kinne I, Tegerstedt G, Falconer C. Sexual dysfunction after trocar–guided transvaginal mesh repair of pelvic organ prolapse. Obstet Gynecol. 2009; 113: 127–133.
- Margulies RU, Lewicky–Gaupp C, Fenner DE, Mcguire EJ, Clemens JQ, DeLancey JO. Complications requiring reoperation following vaginal mesh kit procedures for prolapse. Am J Obstet Gynecol. 2008; 199: 678e1–678e4.
- De Ridder D. Should we use meshes in the management of vaginal prolapse? Curr Opin Urol. 2008; 18: 377–382.
- Diwadkar GB, Barber MD, Feiner B, Maher C, Jelovsek JE. Complication and re–operation rates after apical vaginal prolapse surgical repair. Obstet Gynecol. 2009; 113; Supl 2: 367–373.
- Marcus–Braun N, Theobald P. Mesh removal following transvaginal mesh placement: a case series of 104 operations. Int Urogynecol J. 2010; 21: 423–430.
- Pushkar DY, Vasilchenko MI, Kasyan GR. Necrotising fasciitis after hysterectomy and concomitant transvaginal mesh repair in a patient with pelvic organ prolapse. Int Urogynecol J. 2013; 24: 1765–1767.
- Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber M, et al. Pelvic Floor Disorders Network. Abdominal sacrocolpopexy: A comprehensive review. Obstet Gynecol. 2004; 104: 805–823.
- Kohli N, Walsh PM, Roat TW, Karram MM. Mesh erosion after abdominal sacrocolpopexy. Obstet Gynecol 1998; 92: 999–1004.
- Cundiff GW, Varner E, Visco AG, Zyczynski HM, Nagre CW, Norton PA, et al. Pelvic Floor Disorders Network. Risk factors for mesh/ suture erosion following sacral colpopexy. Am J Obstet Gynecol. 2008; 199: 688. e1–688.e5.
- Stepanian AA, Miklos JR, Moore RD, Mattox TF. Risk of mesh extrusion and other mesh– related complications after laparoscopic sacral colpopexy with or without concurrent laparoscopic–assisted vaginal hysterectomy: Experience of 402 patients. J Minim Invasive Gynecol. 2008; 15: 188–196.
- Bensinger G, Lind L, Lesser M, Guess M, Winkler HA. Abdominal sacral suspensions: Analysis of complications using permanent mesh. Am J Obstet Gynecol. 2005; 193: 2094–2098.
Download






