
MRI in patients suffering from pelvic organ prolapse and stress urinary incontinence
Article authors






Moscow State University of Medicine and Dentistry, Dept. of Urology, Moscow, Russia

Purpose:
The aim of our study was to identify differences in anatomical parameters using MRI in patients suffering from pelvic organ prolapse (POP) according to their continence function.
Materials and Methods:
This study included 44 women suffering from POP (cystocele grade 2-4 by POP-Q) who underwent transvaginal surgical repair. The study was approved by the local ethics committee, and all patients provided signed informed consent. For evaluation of continence, the UDI-6 questionnaire was used. We found that 14 patients (group 1) had concomitant SUI and prolapse. The remaining patients without complaint of SUI were divided into 2 groups: group 2 (n=16) had a negative cough test after prolapse repositioning, and group 3 (n=14) had occult SUI. Dynamic MRI was performed for every patient on MR tomograph General Electric Signa HDxt 3,0 Tesla (Figure 1). The following parameters were recorded: hypermobility of the urethra, dilatation of the bladder neck, retrovesical angle (more than 140°), urethral length, urethral kinking, bladder neck and base descent, uterus descent, cervical elongation, urethral rhabdosphincter thickness, levator gap width and pelvic fascia defect.
Results:
Comparing groups 1 and 2, statistically significant differences were obtained for the dilatation of the bladder neck during Valsalva and for the increase of the retrovesical angle of more than 140° at the Valsalva and at rest was noted (Table 1), which indicates the importance of these factors for continence in patients with pelvic organ prolapse. Statistical analysis did not reveal differences in these parameters between groups 2 and 3. The comparison of groups 1 and 3 also showed statistically significant difference in the same parameter (the increase of retrovesical angle more than 140⁰ only at Valsalva), which may indicate suggests that this parameter might be informative with regard to some information about masking mechanism of occult SUI.
Conclusions:
Patients with POP and SUI have certain anatomical features that should be considered when planning surgical treatment. Further studies on the prognostic significance of these parameters with a large sample are necessary to develop treatment algorithms for this category of patients.
Table 1. Statistically significant differences in parameters of study groups
| Group 1 (n=12) (М±SD) | Group 2 (n=16) (М±SD) | Group 3 (n=14) (М±SD) | p-value | |
| mean±SD | ||||
| Dilatation of the bladder neck during Valsalva, mm | 3.3 ±1.33 | 2±1.46 | 2.54±3.14 | <0.05 |
| Percent (95% confidence interval) | ||||
| The retrovesical angle at the Valsalva of more than 140° | 80% (49.4-100.6) | 43.8% (18.7 -68.9) | 18.2% (5.7-42.5) | < 0.05 |
| The retrovesical angle at rest of more than 140° | 72.7% (38.8-94.6) | 37.5% (13-62) | 52.1% (29.8-74.6) | < 0.05 |
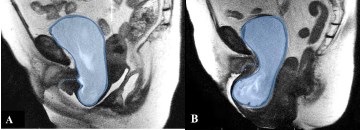
Dilatation of the bladder neck (a), non (b)

POP + SUI
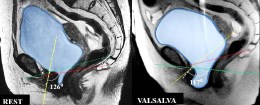
Continent
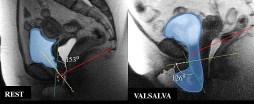
POP + OSUI
Acknowledgement:
The study was funded by the grant of The Ministry of Education and Science, project 14.132.21.1784






