
Transposition of Distal Urethra in Female Patients with Recurrent Lower UTI Associated with Sexual Intercourse
Article authors


1. Introduction
The treatment of recurrent lower urinary tract infections in young female patients remains controversial (Naber, 2000; Stamatiou, 2005; Wagenlehner, 2009). Recurrent lower UTI is often associated with sexual intercourse. The association of UTI with sexual intercourse poses both medical and psychological problems for these patients (Stamatiou, 2005). Usually these patients are young females. Repeated co urses of antibiotic therapy and postcoital antibiotics prophylactic help some, but not a ll patients. Conventional antimicrobial therapy has limited success and often has to be repeated (Naber, 2000). A remarkable increase of antibiotic resistance is also noted in uncomplicated UTI (Wagenlehner, 2009).
“Intravaginal urethral displacement” during se xual intercourse appears to play a role in both the development of these symptoms and the recurrence of UTI symptoms by contamination of microbial agents in the di stal urethra (Stamatiou, 2005), which may often lead to cystitis. The repositioning of the distal part of the urethra may potentially minimize microbial contamination in this area. The op eration makes it possible to withdraw the meatus from the area concerned. Careful mobili zation of the distal part of the urethra with modern technology and fine absorbable suture materials provides minimal invasion and may be considered an option for patients with recurrent UTI associated with sexual intercourse.
In this chapter we shall present detailed surgic al techniques and long-term results of distal urethral transposition in female patients with recurrent UTI associated with sexual intercourse.
2. Methods
2.1 Patients
From 1995 to 2010 two hundred and seventy on e female patients underwent surgical treatment in the Urology Department of MSMS U for recurrent UTI asso ciated mainly with sexual intercourse. The patients ’ age ranged from 16 to 48 years (mean 25.9 years) – Group I. All of them exhibited failure of standard dr ug therapy, including UTI prophylaxis (three- day antimicrobial treatment is recommended for simple cystitis (Valiquette, 2001).All patients had practiced addition al prophylactic methods, such as perineal hygiene, post- coital micturition, with sufficient fluid intake, but with little benefit. The patients themselves also believed that the conservative treatments being used were of little benefit. The mean duration of symptoms before urethral transp osition was scheduled 2,7 years (13 months – 4,5 years). After the failure of traditional medical and conservative therapies (hygiene, antibiotic therapy) all pati ents underwent surgery.
Table 1 shows the age distribution of patients scheduled for surgery.
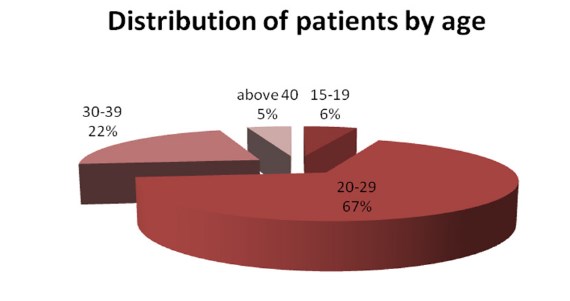
Table 1. Age distribution of pa tients scheduled for surgery.
All patients had long suffered from recurrent infections of the lower urinary tract, mainly from symptoms of acute cystitis. Usually thes e were cases of classic “honeymoon” cystitis. In all cases, the manifestation of the disease coincided with the beginning of regular sexual life. The UTI symptoms were related directly to sexual intercourse, with the duration of recurrences increasing with time and the effici ency of conservative treatment progressively decreasing. It should be noted that sexual sensation became dull in all women, with decreased sexual activity due to the fear of a recurrence of UTI and discomfort in the perineal area.
57 patients (mean age 26, 9) with the same hi stories, anatomical findings, symptoms and signs of lower UTI, receiving conventional antibiotic treatment, served as controls – Group II. Repeated short and long-term courses of antibiotics were used according to urinary culture. It should be noted that this group served as a control for the first year. These patients were advised to have surgery as th ey showed the same anatomical features, but they initially refused to un dergo surgical treatment.
The mean follow up time of the 271 patients fr om Group I was 52.5 months (48 – 57 months). 183 patients were available for additional exam inations after three and five years, (mean 52,5 months).
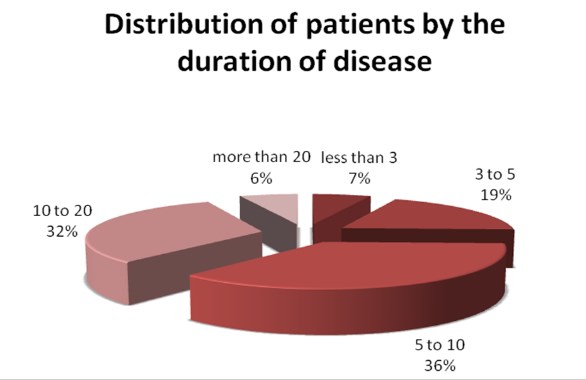
Table 2.
2.2 Preoperative evaluation
Full medical histories were obtained. During vaginal examinations, special emphasis was given to the position of the distal urethra. A plastic penile imitator was introduced vaginally to evaluate urethral movements simulating intercourse. Detailed pelvic examination was described by Hrischhorn in 1966. We believe th at a finger exam and stretching the fingers widely apart does not provide adequate unde rstanding or a complete assessment of the meatal movements. For this reason we decided to use a plastic penile imitator. Urinalysis (including nitrite dipstick an d leukocyte esterase test), urinary culture and urinary tract ultrasonography to exclude anatomical abno rmalities were performed in all patients. Cystoscopy, carried out in all cases, was always normal apart from the occasional finding of urethrotrigonitis. All patients were coun seled extensively regarding anatomy and the technique of this procedure.
2.3 Surgical techniques
This technically simple operation allows the el imination of peculiar «lateral tractions» that permanently displace the meatus into the vagi nal lumen during intercourse and subsequent frictions by causing retrograde infection of the urinary tract by vaginal microflora. The operation makes it possible to withdraw th e meatus from the area concerned and hence create conditions for further ad equate anti-microbal therapy.
The patient is placed in the standard litho tomy position and a conventional cleansing preparation with a sterile covering is used. The procedure starts by analyzing existing urethral-hymenal fusions. In cases where th ese fusions are well-developed, and limit the mobilization of the distal part of the urethr a, they should be dissected widely in the transverse fashion.
In order to mobilize the distal part of th e urethra and create a submucosal bed for subsequent urethral transposition, an inverse te nnis racket incision is performed with a fine 11 blade scalpel. The distal portion of the urethr a should be exposed widely in order to be fixed as close as possible to the clitoral area in the submucosal bed already created. (Fig.1).
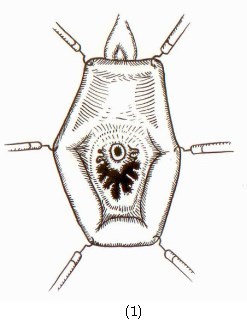

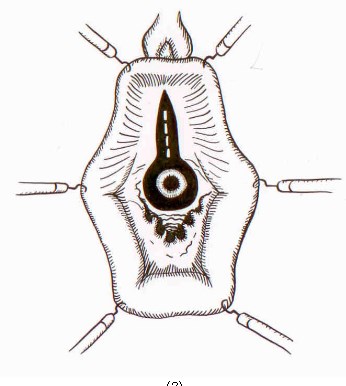
Fig. 1. Incision used for mobi lization of the distal urethra.
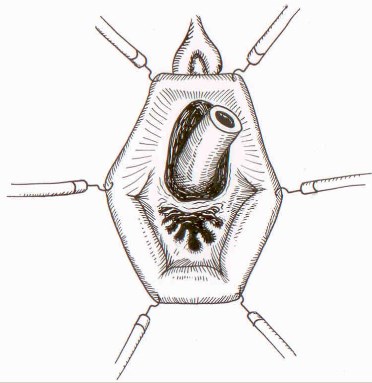
Fig. 2. Exposed distal urethral portion.
The edges of the distal urethra are fixed by interrupted sutures from synthetic absorbable material (Vicryl, Monocryl 4/0) to the tissue of the vaginal vestibule in the formed bed (Fig. 2).
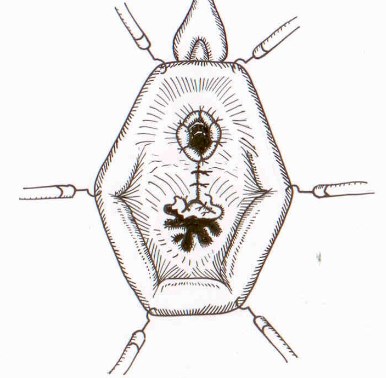
Fig. 3. The initial step of fixing the urethra: the exposed part of the urethral tube is fixed to the apex of the incision.
Sufficient mobilization of the distal part of th e urethra should provide tension-free fixation in the apical part of the submucosal bed. (Fig.3). Tension-free fixation can be achieved by both careful and wide mobilization of the dist al urethra and the sutu ring of previously transversely dissected hyme nal fusions longitudinally.
Care must be taken to provide secure fixation of the external meatus in a new area with the final step of the operation being vaginal mucosa closure.
In cases of vaginal anatomical narrowness, encountered in nulliparas, or marked hymenal ring, the described operation is supplemented by a hymenectomy that enlarges the vaginal orifice and creates the optimal conditions for further sexual life, minimizing bacterial contamination.
2.4 Follow up
A 16 Fr. Foley catheter was placed for three da ys. All patients were treated postoperatively with standard antibiotic therapy course for a mean time of three weeks. Patients were required to avoid sexual interc ourse postoperatively for one month. The mean hospital stay was 2,6 days.
3. Results
Patients from Group I were evaluated afte r three months, showing no postoperative complications. Those who wished to begin sexual activity were able to do so after one month. Coital activity was resumed with no further recurrence of pre op. dyspareunia. Examinations of 204 (75,3%) patients from Gr oup I one year later showed no symptoms and signs of UTI. 67 (24,7%) patients required further antimicrobial prophylaxis after the procedure because of the longer preoperative du ration of their symptoms. 19 patients (7,1%) showed poor results. 183 patients were availabl e for additional examinations after three and five years, (mean 52,5 months) revealing stable results with no lower UTI for these patients. It should be noted that the flow rate remained unchanged postoperatively, with no signs of obstruction or dysfunctional voiding. Patients did not complain about sexual dysfunction postoperatively, although it should be noted th at we did not conduct in-depth evaluations. Group II patients were followed up for one ye ar. 46 (80,7%) of them were found to have recurrent symptoms with poor response to the therapy, and had to undergo repeated treatment.
4. Discussion & conclusion
Recurrent UTI and dysuria associated with sexual intercourse represent a common urological problem. The relationship of lower ur inary tract symptoms with sexual activity is well recognized in terms of onset and recurrence. This condition automatically leads to dyspareunia (Valiquette, 2001).
It seems that distal urethral vaginal ectopy with intravaginal movements of the external meatus during sexual intercourse plays an im portant role in the development of acute UTI with symptoms of acute cystitis (Reed, 1970) . The antimicrobal defense mechanism of the urethra is altered by frequent recurrences, and conventional antimicrobal therapy may not help. Careful physical examination may provid e a detailed evaluation of distal urethral position and assess urethral-hymenal fusions. Initial work done by Hirshhorn in early 1966 concluded that bilateral hymenotomies may provide a stable effect with no further recurrence of urethritis or cyst itis (Hirshhorn, 1966). This type of procedure has been used in our department for many years with limited success. We feel that simple finger evaluation of the distal urethra movements will not provide adequate information in order to select candidates for surgery. We have developed a simple method of assessment of the urethral position by simulating sexual intercourse with a plastic penile imitator. We now believe that all younger sexually active females who develop dysuria after sexual intercourse should be evaluated by this method in order to exclude in travaginal movements of the distal urethra. In 1972 Alan R. Alexander et al. published a limited study on bilateral hymenectomy alone or with urethral transposition, achieving good results (Alexander et al, 1970). They considered urethral transposition a radical op eration which should be reserved for only those cases in which the patients failed to re spond to simple bilateral hymenectomy. We may understand that at that time there was not such a wide variety of antibiotics. Therefore some cases could have benefited from simple bilateral hymenectomy. We now try to prescribe longer courses of antibiotic treatm ent with stronger agents. We may therefore assume that our patients would not benefit from a simple bilateral hymenectomy.
Careful mobilization of the distal part of the urethra with modern technology and fine absorbable suture materials provides minimal in vasion and may be considered an option for patients with recurrent UTI associated with sexu al intercourse. It shou ld be emphasized that we do not advocate this procedure as a primar y choice. This means that all patients showing this type of UTI should be initially treated co nservatively, and scheduled for surgery only if this treatment is unsuccessful.
5. References
Alan R. Alexander, Paul M. Morrisseau – Urethral-hymenal adhesions and recurrent post- coital cystitis: treatment by hymenoplasty . The Journal of Urology, Vol. 107, April 1970 Hirschhorn R. C. Urethral - hymeneal fusion: a surgically correctable cause of recurrent cystitis. Obstetrics and Gynecology. Vol. 26, No 6, 1965. pp. 903 - 908.
Naber KG. Treatment options for acute uncomplicated cystitis in adults. Urological Clinic, Hospital St Elisabeth, Straubing, Germ any. J Antimicrob Chemother. 2000 Sep;46 Suppl 1:23-7; discussion 63-5
Reed J. F. Urethral - hymenal fusion: a cause of chronic adult female cystitis. The Journal of Urology. 1970, vol. 103, No 4 pp. 374 - 378.
Reziciner S. Prevention of recurrent post-coital cystitis using hymenoplasty. Ann Urol (Paris). 1988;22(6):446-51
Santucci RA, Payne CK, Saigal CS – Office dilatation of the female urethra: a quality of care problem in the field of urology. J Urol. 2008 Nov;180(5):2068-75.
Scotti R. J. Ostergard D. R. The urethral syndrome. Obstetrics and Gynecology Vol. 27, No 2, pp. 515 - 529.
Smith PJ, Roberts JB, Ball AJ – “Honeymoon cyst itis” : a simple surgical cure. BJU, 1982, 54, 708-710 Stamatiou C, Bovis C, Panagopoulos P – Sex-induced cystitis – patient burden and other epidemiological features. Clin Ex p Obstet Gynecol. 2005;32(3):180-2.
O’ Donnell R. P. Relative hypospadias potentiate d by inadequate rupture of the hymen. Int. Coll. V 32, p 374 - 388. 1959.
Valiquette L. – Urinary tract infections in women. Can J Urol. 2001 Jun; 8 Suppl 1:6-12






